This week is Te wiki o te Reo Māori, what better time to introduce you to two Māori rehabilitation tools that are used at ABI. Both of these tools are authored by Dr Hinemoa Elder (Ngāti Kurī, Te Rarawa, Te Aupōuri and Ngāpuhi) a Child and Adolescent and Forensic Psychiatrist.
Some key aspects of these models include:
- The role of whānau is deemed an essential aspect of hauora (wellbeing) by Māori who are over-represented in brain injury (either by accident or medical event).
- Whānau mātauranga (family knowledge systems) can greatly improve recovery outcomes for those with such injuries.
- An injury to the brain also is an injury to wairua, not just for the injured person, but their whānau and whakapapa wairua – a medical and cultural injury.
- The head and brain in Te Ao Māori is sacred and tapu.
- The importance of Te Reo Māori in these tools.
Te Waka Kuaka and Te Waka Oranga
These models empower whānau to sit alongside clinicians to collectively guide the waka towards the agreed destination. The clinical team must sit in a Māori space and is likened to a team of paddlers working together to move the waka forward.
Te Waka Kuaka
Te Waka Kuaka is a bilingual cultural needs assessment tool for whānau.
Te Waka Kuaka means a flock of godwits, who are renowned for their long distant migration. Te Waka Kuaka helps whānau to organise their thinking to identify their needs in order to better navigate their healing journeys, much as the godwits organise themselves in order to navigate their long distance migrations.
The four navigational priorities that form the assessment subscales are helpful in grouping areas of focus:
- Wairua;
- Tangata (people);
- Wā (time); and
- Wāhi (place).
The whānau are asked to rate the importance of statements in relation to healing. The responses can then be reviewed by the clinical team to review what are the needs and priorities for the whānau. This in turn supports a far more culturally responsive rehabilitation plan.
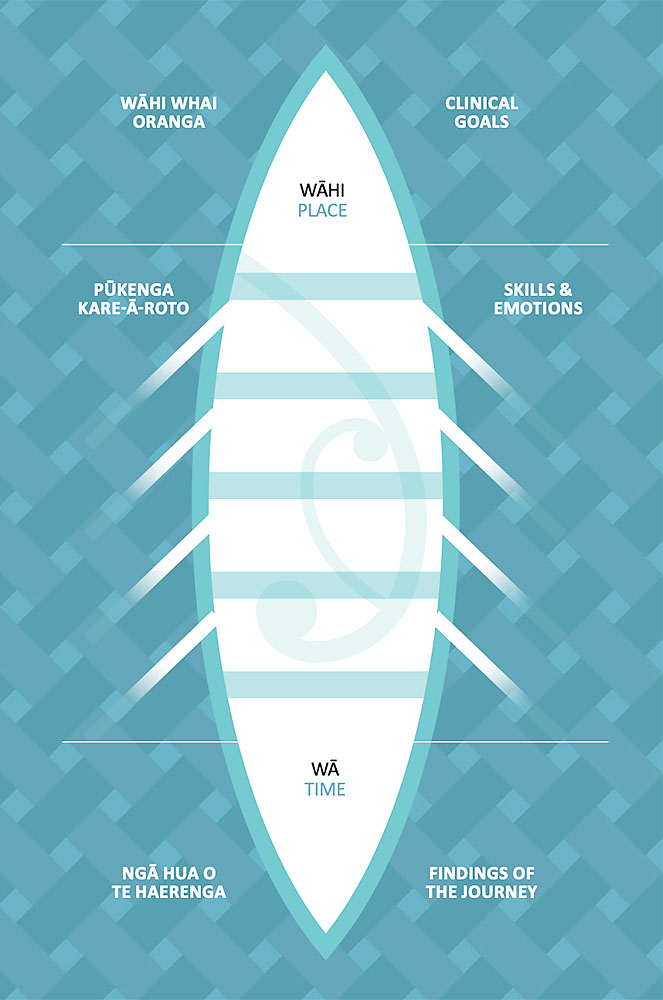
Te Waka Oranga uses the metaphor of a waka and is looked down from the sky above by the kuaka. Whānau and the clinical team are paddling together equally, to bring forward the recovery destination. Bringing together whānau, their knowledge, skills, and feelings, with the clinical team’s knowledge, skills, and feelings to improve the experience of recovery and reach that destination.
Te Waka Oranga is jointly paddled and navigated; culturally and clinically.
There are 2 stages within this rehabilitation model
- Hoe tahi: Paddling as one. Establishing the ground rules of Te Waka Oranga. Who is on board paddling. Each paddle has a skills side and an emotional side. Use of whakatau or pōwhiri. Completion of Te Waka Kuaka and using the insights from this. Consideration of head and brain as tapu, the impact of injury on wairua of the individual, the whānau and the whakapapa. Acknowledgement of the place where rehabilitation is taking place (ie a long way from marae) and other mutually agreed protocols.
- Te Haerenga o te Waka Oranga: Launching, sailing and arriving. Implementing the agreed processes in “hoe tahi” into action for the rehabilitation journey. The launching and sailing requires collaboration, skill sharing and high quality communication and connection to one another. Different parts of the overall rehabilitation journey can be divided up into shorter journeys providing for flexibility when thinking about the destination so as to make the journeys (and goals) achievable.
The teams using these models feel their connection with the client and whānau is greatly strengthened. Whānau have felt respected, included and equal partners in the journey.

Reference: Elder, H. Te Waka Kuaka and Te Waka Oranga. Working with Whānau to Improve Outcomes. Australian and New Zealand Journal of Family Therapy, 2017; DOI https://doi.org/10.1002/anzf.1206